Michigan Medicaid is making major changes to coverage for GLP-1 medications like Wegovy® and Zepbound®—and thousands of patients may soon lose access. Beginning in late 2025, coverage will tighten to focus only on those with higher BMIs or qualifying medical conditions, leaving many individuals unsure whether their treatment will continue. This comprehensive guide explains what’s changing, why it’s happening, and how Life IV Weight Loss is helping patients navigate renewals, appeals, and safe alternatives.
Last Updated on November 13, 2025 by justin@lifeivtherapy.com
Understanding Michigan Medicaid’s New GLP-1 Coverage Rules
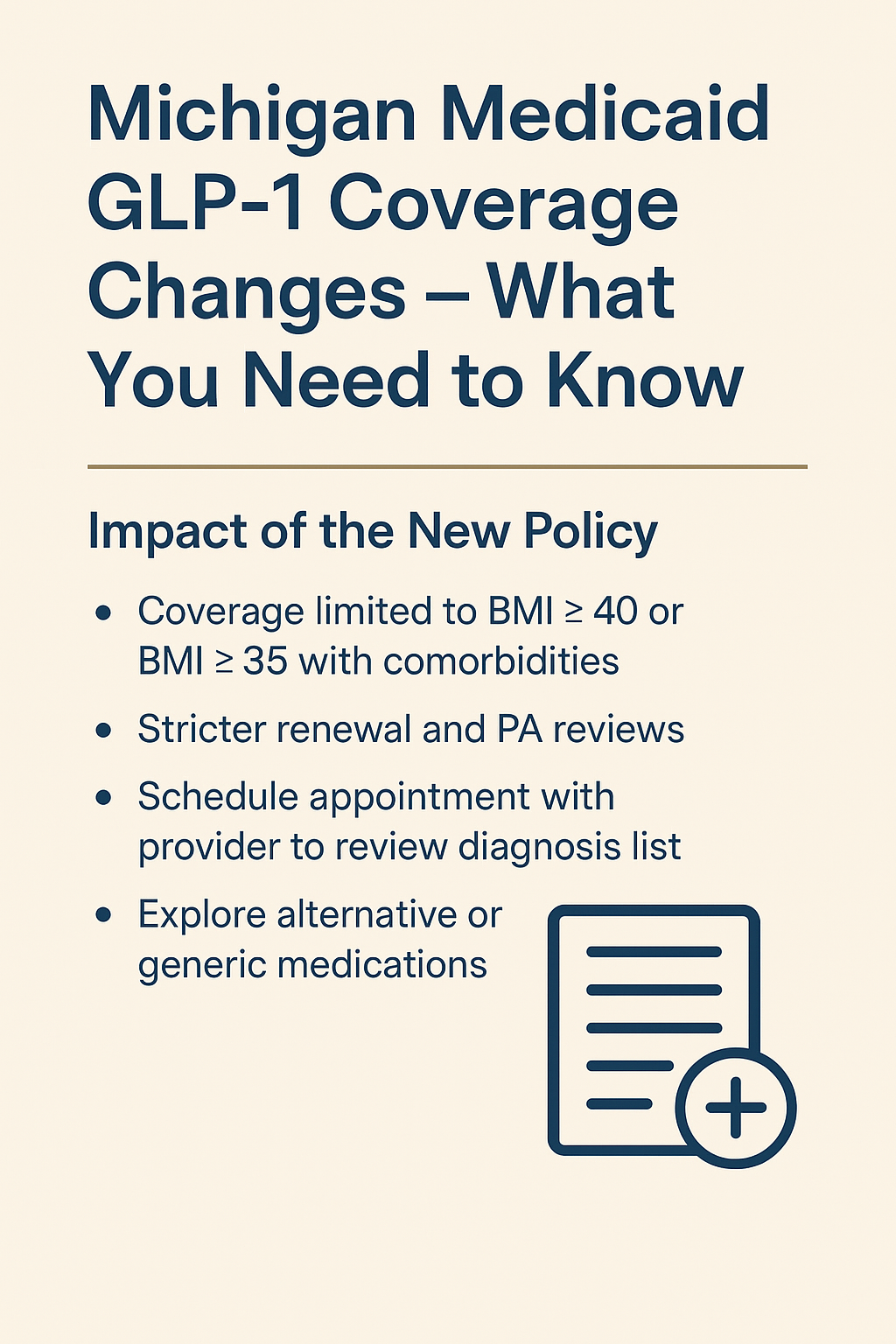
In late 2025, Michigan Medicaid will implement significant restrictions on coverage for GLP-1 receptor agonists used for weight loss—including brand-name medications such as Wegovy® and Zepbound®. Eligibility will now prioritize patients who are medically classified as having Class III obesity (BMI ≥ 40 kg/m²) or Class II obesity (BMI ≥ 35 kg/m²) with serious comorbidities (such as diabetes or sleep apnea). Patients below these thresholds may lose coverage unless additional qualifying diagnoses are documented.
These changes follow similar nationwide trends as states manage rising prescription drug expenditures. GLP-1 medications—though effective—are among the costliest long-term pharmaceutical interventions in modern healthcare. With more than 200,000 Michigan Medicaid beneficiaries considered medically eligible for obesity treatment, the state legislature and MDHHS have moved toward stricter criteria to contain costs, especially in the face of growing demand (Bridge Michigan, 2025).
This shift has long-term implications for patients, providers, pharmacies, and weight-management clinics. Understanding the new rules is the first step toward protecting your access to treatment.
Why Michigan Medicaid Is Restricting GLP-1 Coverage
Michigan is not alone—over a dozen states have already implemented stricter GLP-1 criteria for Medicaid recipients. The decision is driven by a combination of economic, clinical, and legislative factors. CBS Detroit reports that the updated policy is expected to save Michigan Medicaid nearly $240 million annually (CBS Detroit, 2025). Even though GLP-1 medications offer life-changing benefits, they represent a major financial strain on public health programs.
Key Drivers Behind the Policy Change
- Rising program costs: GLP-1s can cost $900–$1,300 per month per patient without insurance coverage. Medicaid covers this expense when prior authorization criteria are met.
- Escalating demand: Since 2023, prescriptions for GLP-1 medications have increased dramatically nationwide as they gained popularity for weight loss.
- Limited long-term data for lower-BMI patients: Medicaid programs often require stricter justification for treatments lacking decades-long outcome research.
- Legislative pressure: State lawmakers face pressure to reduce spending on specialty drugs to protect Medicaid budgets.
The state’s official position is not to remove access entirely but to ensure that coverage is “clinically appropriate and cost-effective.” That means only patients meeting higher medical-necessity thresholds will remain approved for GLP-1 therapy under Medicaid.
Who Will Still Qualify for GLP-1 Coverage?
Under the revised criteria, Michigan Medicaid will continue coverage for GLP-1 weight-loss medications for individuals who fall into one of two categories:
1. Patients With Class III Obesity
Defined as:
- BMI ≥ 40 kg/m²
This group represents the highest-risk population for obesity-related complications, making continued coverage more medically justified.
2. Patients With Class II Obesity and Serious Comorbidities
These include:
- Type 2 diabetes mellitus
- Obstructive sleep apnea
- Hypertension
- Dyslipidemia
- Non-alcoholic fatty liver disease
Michigan Medicaid’s updated clinical guidelines mirror the state’s existing requirements for bariatric surgery coverage, which similarly use BMI thresholds and comorbidities as qualifying criteria (MDHHS, 2023).
Patients Likely to Lose Coverage
Patients may face coverage disruption if they:
- Have a BMI below 35 kg/m²
- Do not have a documented qualifying comorbidity
- Have incomplete or outdated chart documentation
- Miss renewal deadlines or prior authorization re-submissions
For these patients, timely chart updates and proper medical documentation can be the difference between continuation and denial.
How Prior Authorization (PA) Requirements Will Change
Michigan Medicaid will implement tighter renewal and documentation requirements for all GLP-1 prescriptions. The handout notes that PA reviews will become “more stringent,” requiring more detailed evidence of medical necessity and patient progress.
What Payers Will Now Require
- Updated weight and BMI measurements
- Documented lifestyle changes and adherence to treatment
- Evidence of beneficial response to therapy
- Up-to-date comorbidity diagnoses in the medical record
- Proof that the medication continues to be medically necessary
Stricter Ongoing Monitoring
Expect payers to require:
- More frequent follow-up visits
- Updated chart notes for each renewal
- Standardized metabolic labs
Gaps in follow-up or incomplete documentation could lead to denials—even for medically qualified patients.
How This Policy Impacts Patients in Michigan
The new rules may affect thousands of Medicaid recipients currently using GLP-1 medications. Understanding these impacts can help patients prepare and protect their access to care.
1. Many Patients Will Need New Documentation
Patients should schedule appointments ASAP to update:
- Diagnosis lists
- BMI and weight records
- Comorbidity documentation
- Past medication failures
2. Some Individuals May Experience Coverage Loss
Individuals with BMI below 35 kg/m² or those without major comorbidities may receive denials once the new policy takes effect. It is critical for patients to discuss alternative treatment paths with their provider to avoid interruptions.
3. Appeals Will Become More Common
Medicaid decisions are appealable, but supporting documentation must be strong, clear, and medically justified.
4. Medication Access May Shift Toward Non-Brand Options
Patients could be transitioned to:
- Generic medications (when available)
- Off-label metabolic therapies
- Medically supervised weight-management programs
5. More Follow-Ups Will Be Required
Expect more frequent follow-up appointments to maintain eligibility and supply updated documentation.
How Life IV Weight Loss Helps Patients Navigate These Changes
Life IV Weight Loss is already preparing patients for the new Medicaid rules. As the handout states, our clinic will continue to support clients by providing documentation, helping with renewals, managing appeals, and guiding patients toward safe alternatives when needed.
1. Comprehensive PA Documentation
We handle:
- Accurate BMI and medical history documentation
- Comorbidity verification
- Detailed clinical notes to support PA approvals
- Submission of updated metabolic labs
2. Appeal Support When Coverage Is Denied
Our team:
- Reviews reason for denial
- Gathers missing documentation
- Submits detailed appeal letters including clinical rationale
3. Exploring Safe Medication Alternatives
We help patients navigate:
- Pharmaceutical alternatives
- Evidence-based non-GLP-1 options
- Affordable treatment alternatives
4. Transparent Communication and Patient Advocacy
We keep patients informed with:
- Policy updates
- Renewal reminders
- Educational materials
5. Seamless Scheduling and Access
With our new Tecumseh, Michigan location, flexible hours, and returning provider, we make access easy for patients managing multiple health needs.
What Patients Should Do Right Now
To prepare for the policy change, patients should take the following steps immediately:
✔ 1. Schedule a Chart Review Appointment
Meet with your provider to review and update your diagnosis list, BMI, weight history, and comorbidity documentation.
✔ 2. Ensure Comorbidities Are Properly Documented
If you have diabetes, OSA, hypertension, or dyslipidemia, it must be clearly coded in your chart to qualify.
✔ 3. Request Copies of Prior Medical Records
Previous diagnoses may strengthen your PA renewal.
✔ 4. Verify Your Medicaid Plan’s Specific Requirements
Plans under the Medicaid umbrella (Meridian, Molina, Priority Health Medicaid, etc.) may have nuanced differences.
✔ 5. Keep Up With Follow-Up Appointments
Missed visits are a common reason for denial.
Alternatives for Patients Who Lose Coverage
If you no longer qualify for GLP-1 coverage, several safe and clinically supported alternatives exist. Life IV Weight Loss helps patients explore options based on their health profile, goals, and financial needs.
Alternative Prescription Therapies
Depending on your medical history, options may include:
- Metformin (especially beneficial for insulin resistance)
- Bupropion-naltrexone
- Phentermine
- Topiramate-based regimens
Research shows several non-GLP-1 therapies offer meaningful weight-loss support when used with structured programs (Apovian et al., 2022).
Behavioral and Lifestyle Interventions
- Calorie-tracking programs
- Structured nutrition plans
- Exercise programming tailored to weight-management goals
At Life IV Weight Loss, these align with the 4 Pillars of Weight Loss developed by Dr. Victor Cherfan: motivation, calorie restriction, calorie tracking, and medication.
Out-of-Pocket Options Through Low-Cost Pharmacies
We help patients compare cost-saving programs, generic options, and non-insurance solutions when available.
Safe Decline After Medication Discontinuation
Stopping GLP-1 therapy should be medically supervised to avoid rebound weight gain. We develop personalized tapering and maintenance strategies.
Frequently Asked Questions (FAQ)
Will I automatically lose coverage?
No. Patients meeting the new criteria will continue to qualify. However, failure to update documentation can result in denial.
Does Michigan Medicaid still cover GLP-1 medications for diabetes?
Yes. Diabetes coverage criteria are separate and remain intact.
When do the changes take effect?
Late 2025, exact date is unknown.
Can I appeal a denial?
Yes. Life IV Weight Loss assists with medically appropriate appeal submissions.
Will commercial insurance plans follow Medicaid?
Some already have. Coverage tightening is becoming a nationwide trend.
Conclusion: Protecting Access During a Time of Change
Michigan Medicaid’s new GLP-1 coverage rules represent one of the biggest policy shifts in the history of medical weight management. While many patients may continue to qualify, thousands may face new barriers—making proactive documentation, follow-up care, and advocacy more important than ever.
Life IV Weight Loss is committed to defending patient access, supporting appeals, offering alternative therapies, and guiding individuals through every step of this transition.
If you are concerned about your coverage, schedule your appointment now so we can safeguard your treatment plan before the new Medicaid rules take effect.
References
- Bridge Michigan. (2025). Michigan cuts off weight-loss drugs for most Medicaid patients, saving $240 million.
- CBS Detroit. (2025). Michigan to limit Medicaid coverage for weight loss drugs to people with diabetes and those ‘morbidly obese.’
- Michigan Department of Health and Human Services. (2023). BMI criteria for weight-loss surgery coverage in Michigan Medicaid.
- Apovian, C. et al. (2022). Pharmacologic treatment of obesity: mechanisms, efficacy, and clinical considerations. New England Journal of Medicine.
- American Diabetes Association. (2023). Standards of Medical Care in Diabetes.